Oncology
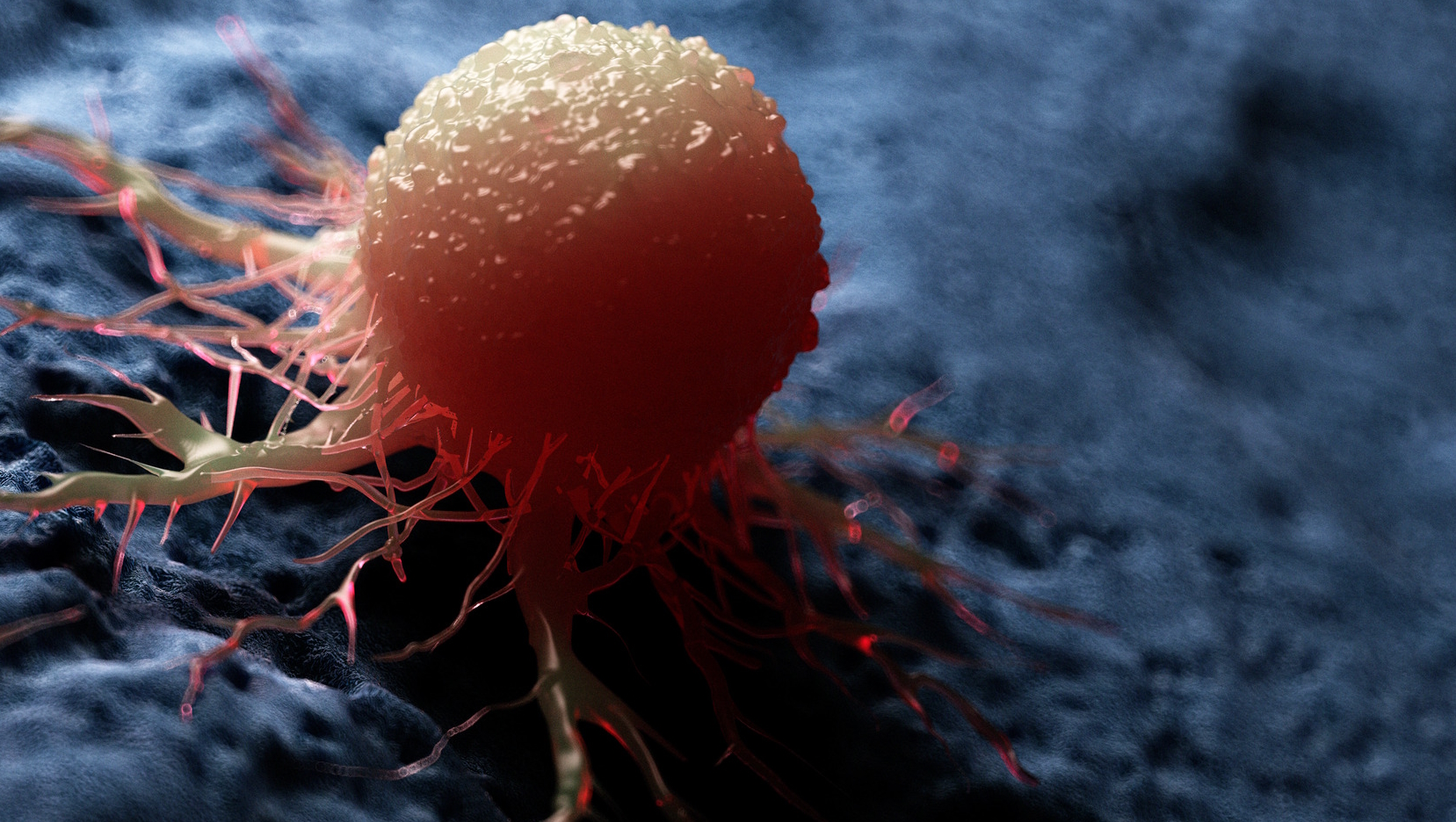
Oncology is a critical branch of medical research that specialises in the treatment and diagnosis of cancer.
Cancer is a complicated and multidimensional disease that can spread to other parts of the body and is characterised by unchecked cell growth brought on by genetic or epigenetic changes.
Since cancer typically manifests itself in an unexpected manner with a variety of symptoms, important aspects of its uncontrolled cell growth, tumour formation, metastasis, or underlying genetic mutations are still being studied and researched.
In order to reduce the number of deaths and suffering caused by various cancer causes each year, researchers and pharmaceutical R&D have been working to develop therapies, diagnose problems, and understand or stop the recurrence of malignant tumours.
.jpg?width=50)
2BScientific Limited, the UK and Ireland's leading distributor in life science reagents are committed to helping researchers, pharma R&D and CRO enhance their research capability by offering range of cancer products provided by our suppliers from offering:
- Highly validated antibodies for tissue staining for cancer histopathology
- Checkpoint proteins and Inhibitors for cancer immunotherapy and in-vivo research
- Range of microarrays and Antibody panels to understand Tumour Microenvironments (TME)
- Develop cancer models to utilise in your cell culture research
- Deliver or insert genes using CRSIPR/Cas9 technology and using CAR-T for development
- Using biopsy to isolate Extracellular Vesicles that can determine cancer diagnosis
- Uncovering post translational or genetic modifications through protein screening using assays, arrays and antibodies for phosphorylation, methylation, ubiquination, glycosylation.
2BScientific Limited has a range of products, including a selection of cancer research-based products. 2BScientific is passionate about ensuring that customers get the precise, required product and have a friendly and knowledgeable team ready to answer any technical queries.
